PT Solutions
Management of Cervicogenic Dizziness Using Vestibular Rehabilitation and Manual Therapy: A Case Series on Diagnosis and Treatment
September 18, 2013
Management of Cervicogenic Dizziness Using Vestibular Rehabilitation and Manual Therapy: a Case Series on Diagnosis and Treatment
Lindsay W. Sarbeck, PT, DPT
STUDY DESIGN: Retrospective clinical case series OBJECTIVE: To evaluate the effectiveness of the management of three patients with cervicogenic dizziness using manual therapy, cervical proprioception, and home exercises. BACKGROUND: Cervicogenic dizziness is now commonly accepted amongst medical professionals as a true anatomical pathology. However, once a diagnosis has been made, little is known about the course of rehabilitation for this condition. CASE DESCRIPTION: A series of three patients (ages 17, 18, and 65) were referred to an orthopedic therapist for cervical spine pathology with varying mechanisms of injury. All patients also reported dizziness or unsteadiness with neck movement. Numeric pain rating scale, visual tracking, cervical range of motion, the Romberg test, and cervical proprioceptive accuracy were assessed at initial examination and discharge. Interventions included: manual therapy to the upper thoracic and cervical spine, scapular strengthening, cervical proprioceptive exercises, and a home program (including vestibulo-ocular reflex exercise progression). The patients were seen for 16 to 20 sessions. OUTCOMES: All three patients had substantial improvement in NPRS and cervical ROM scores. DISCUSSION: A multimodal approach for patients with cervicogenic dizziness may be useful for this diagnosis to reduce pain, minimize dizziness symptoms, and improve functional outcomes. LEVEL OF EVIDENCE: Level 4 KEY WORDS: cervicogenic dizziness, concussion, vestibular rehabilitation, and manual therapy
Introduction
Dizziness is a frequent complaint seen by the primary care physician, comprising 2.6% of visits. Because of its multiple contributing systems and reliance on subjective data, dizziness can be very frustrating and mystifying for the diagnosing health care provider. This is particularly true in the diagnosis of cervicogenic dizziness, which involves both central and peripheral vestibular systems, as well as proprioceptive input from the cervical spine. Cervicogenic dizziness is defined as: “a non-specific sensation of altered orientation in space and disequilibrium originating from abnormal afferent activity from the neck.”12 Once considered a phony diagnosis, cervicogenic dizziness is now more accepted among medical professionals as a legitimate diagnosis. However, once a diagnosis has been made, little is known about the course of rehabilitation for this condition.
There is a complex array of anatomical structures in the cervical region providing the brain with information of head and neck position sense (HNPS). These areas are closely integrated with the vestibular system. It is largely decided that the muscle spindle is the primary receptor responsible for joint position sense. Within the neck muscles, mainly the intertransverse and centrotransverse intervertebral muscles, exists a high density of muscle spindle fibers. 1 Joint position sense in the cervical spine can be altered by vestibular disorientation, creating abnormal head righting. It is proposed that the opposite could be true as well; injury to the joint position sensor system created by whip-lash trauma or spondylogenic changes can signal abnormal vestibular input to the central nervous system.6 Researchers have found that injecting anesthetic into the dorsal roots of the cervical spine in humans can create disequilibrium towards the injected side, with strong feelings of unsteadiness. Wapner also discovered that a sense of tilting or falling can be created by electrical stimulation to the cervical musculature in humans. 11It is proposed then, that rehabilitation of cervicogenic problems should attempt to re-establish a more symmetrical and normal proprioceptive feedback from the muscle spindles of the cervical spine to the central nervous system.
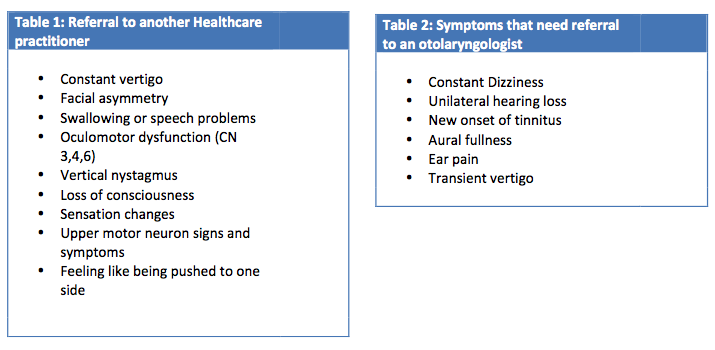
Cervicogenic dizziness or cervical vertigo is commonly seen in physical therapy patients with associated neck pain, limited range of motion, headaches, and nausea. Because cervicogenic dizziness is a diagnosis of exclusion, it is imperative for the physical therapist to (1) determine whether referral to another medical practitioner is warranted, (2) take a thorough subjective history to understand the pathophysiology and mechanism of injury, and (3) identify the relationship between dizziness and other neck objective findings. Current subjective information that may be indicative of cervicogenic pathology includes: a mechanism of trauma to the neck, history of cervical degenerative disease, dizziness lasting between hours and days, dizziness related to certain head movements, headaches, and general unsteadiness. Refer to Table 1 and 2 for a list of red flags that would warrant referral to another healthcare provider.
While increasing literature exists to support the diagnosis of cervicogenic dizziness, there is still limited evidence in the physical therapy management of patients with these conditions. Some literature describes the use of a combination of manual treatment with vestibular rehabilitation techniques for management of these patients. 4,10 This is intuitive, as patients with cervicogenic dizziness may have mechanical impairments of the cervical spine, as well an abnormally functioning vestibular system. Both of these impairments can contribute to abnormal head and neck position sense. While it is commonly accepted to integrate proprioceptive exercises into the management of lower extremity injuries, this has not been true for the treatment of cervical injuries. The purpose of this case study looks to demystify the nature of cervicogenic dizziness and describe the physical therapy treatment and outcomes of three patients using cervical proprioceptive training and manual therapy techniques.
Case Descriptions
Patients were referred by their primary care physicians to an outpatient orthopedic clinic. They were diagnosed with either neck or shoulder pathology. All patients underwent a history intake and physical therapy examination. History included: reviewing medical history, medications, prior surgical history, systems review, and current subjective presentation. The physical examination included screening for red flag conditions, as well as objective tests and measures for cervical and vestibular dysfunction.
Case 1
The first patient with cervicogenic dizziness is an 18-year-old female competitive aerialist. She has no significant prior medical history or surgical history. At the time of evaluation, her symptoms consisted of dizziness, chronic headaches, and scapular pain, since sustaining a concussion five months prior. Mechanism of injury occurred as Case 1 was performing an aerial stunt when she fell eight feet, landing on her head and left shoulder. After falling, she went to the emergency department, underwent x-ray imaging determined to be negative for fracture, and was sent home on rest. Her pain on the Numeric Pain Rating Scale (NPRS) was 7/10 at the time of evaluation. Her goals included being able to read without headaches, and return to aerial stunting.
Case 2
Case 2 is a 17-year-old, male high school football player who sustained a concussion at a football game one week prior to evaluation. Case 2 recalls hitting another player with his head during the game, falling to the ground, and then experiencing “tunnel vision” upon standing. He denied having loss of consciousness. After his injury, Case 2 went to the emergency department where received cervical x-rays and a MRI defined as normal, and then he was sent home with instructions for cognitive rest. His primary care physician also referred him to physical therapy for neck and shoulder pain. At the time of evaluation, he denied any significant prior medical history or prior surgical history. His chief complaints consisted of dizziness, unsteadiness, headaches, nausea, and 7/10 neck pain on NPRS. His goals included returning to school, decreasing neck pain, and playing football.
Case 3
Case 3 is a 65-year-old female patient with chronic torticollis of the left sternocleidomastoid, beginning three years ago. She reports having hypertension but no other significant medical history. Her medications include: Lisinopril, Crestor, Aspirin, Baclofen, and Paroxetine. Her chief complaints consisted of: falling, sinus pressure, headaches, disequilibrium, difficulty reaching overhead, and 6/10 pain on the VAS. Her goals were to decrease her pain and reduce her fall risk. At the time of evaluation, she reported having multiple falls, as well as severe unsteadiness and running into objects when her neck began to spasm.
Clinical Impression
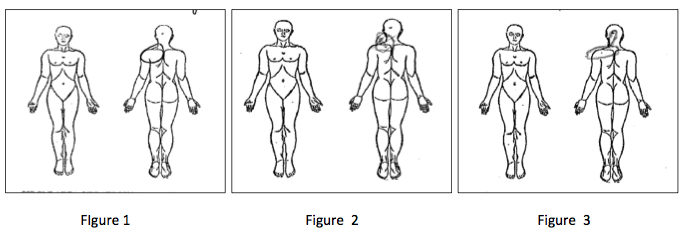
While these three cases may vary in their initial clinical presentation, all subjects described having the same location of pain in the left posterior shoulder and neck on their initial in-take forms. Refer to Figures 1,2, and 3 below for the pain diagrams of the each case respectively. Also of significance is the size or area in which they circled on the pain diagrams. Finally, it is noteworthy that all patients reported a rather high intensity of pain on the visual analog scale (6-7/10). It is suggested that this subjective information, in combination with symptoms of dizziness, could be very useful in diagnosing patients with cervicogenic dizziness. However, subjective pain location is not typically considered a reliable diagnostic tool.7 There are several potential structures that could be contributors to this posterior shoulder pain including, but not limited to: the upper trapezius and levator scapula, the lung and diaphragm, C5-7 facet joint, and supraclavicar and cervical cutaneous nerve roots. The spinal accessory nerve is primarily responsible for motor function in this region, and also contains non-proprioceptive sensory and pain fibers.8 It is not clear the significance that these anatomical structures have with the onset of cervical dizziness but is proposed that treatment of this area may be effective and further research is warranted.
Examination
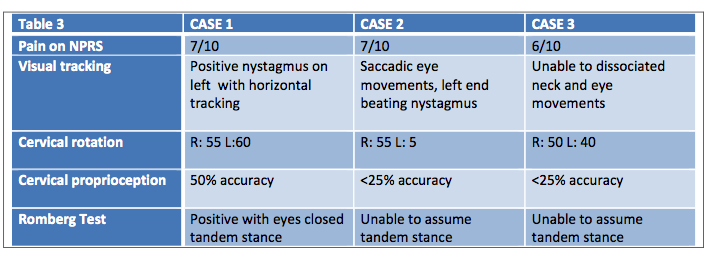
The diagnosis of cervicogenic dizziness is mostly a diagnosis of exclusion, meaning that other central nervous system or vestibular pathology should be ruled out. There are few tests of poor reliability that are currently available to diagnose patients with cervicogenic dizziness. 2-7 Performance of a complate orthopedic and neruologic exam could lead to a very time consuming and exhaustive examination process for both the patient and the therapist. Therefore, it is proposed that, in combination with subjective complaints of cervical pain with non-specific dizziness, the following objective tests should be performed if cervicogenic dizziness is suspected: visual tracking, cervical rotation range of motion, cervical proprioception, and the Romberg test. Other vestibular tests may be performed such as the head-thrust, or dix-hallpike maneuver if peripheral vestibular involvement is suspected. However, subjects may receive a false-positive on these assessments, as they involve cervical motion.
Visual tracking: in unsupported sitting, the subject holds their head stationary while following an examiner’s finger with their eyes, tracking 30 degrees to the right, left, up, and down briefly pausing at end points to observe nystagmus. Therapist observes for any saccadic eye movements with tracking.
Cervical rotation AROM: in unsupported sitting, instruct the subject to actively rotate the head to end range right and left rotation. Observe eyes for any nystagmus, and ask patient if rotating their head increases their symptoms. It is important for the therapist to recall that at least 45 degrees of rotation and 30 degrees of extension is needed in the cervical spine before ruling in/out peripheral involvement using the Dix-Hallpike maneuver. The minimal detectable change for outcomes varies between 5 and 10 degrees for each direction.11
Cervical proprioception: in supported sitting, have patient sit four feet away from target. Fix laser to subject, and align their head and neck in neutral, with laser pointing in middle of target. Instruct subject to close their eyes, rotate their head to right with eyes closed to a tolerated end range. Then have the subject return to their suspected neutral and visually assess distance from target. Repeat for the left side, for three trials each. Accuracy was assessed using four-ringed target, with 100% accuracy aiming towards the center of the target, 75% being within the first two rings, 50% in the first three rings, and 25% remaining on the page.
Romberg test: Have the subject assume tandem stance; if they cannot, have them put feet together. Instruct the patient to sequentially place their arms across their chest, close their eyes, and extend their head backwards to tolerance. Record time the subject sustains the position without loss of balance. Objective data is listed below in Table 3.
Intervention
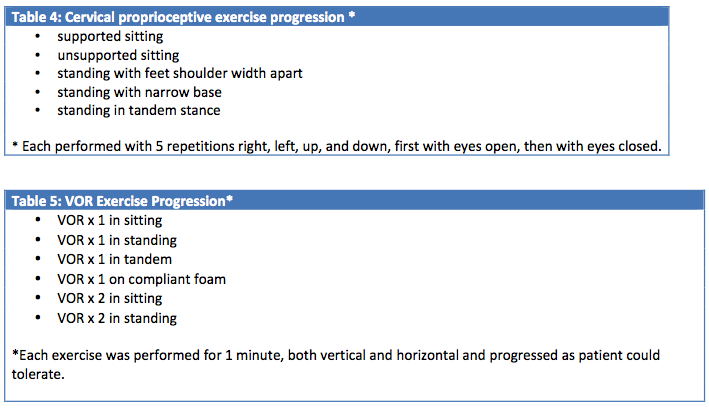
Because cervicogenic dizziness involves multiple systems, a multi-disciplinary approach to treatment was utilized. Manual therapy interventions included: soft tissue work to the sternocleidomastoid, scalene, and levator scapula, and deep trigger point pressure to the C5-6 facet joints. Supine thoracic and cervical thrust manipulations were used in Cases 1 and 2. Cervical proprioceptive exercises were also incorporated using feedback from a laser device to work on mid-line orientation and fine motor movements of the head on the neck. All patients were given a home exercise program of vestibulo-ocular reflex (VOR) exercises. See below Tables 4 and 5 for detailed progression of cervical proprioceptive and VOR exercises. All treatment interventions were tailored to individual’s needs and specific musculoskeletal and vestibular impairments. For instance, in order for Case 1 to return to aerialist activity, emphasis was placed on scapular endurance and performing vestibular habituation exercises in inverted positions. In order for Case 2 to return to playing football, more emphasis was spent on building strength and power of scapular and cervical stabilizers, and balance training with quick head rotations. Much of the emphasis of treatment for Case 3 included improving safety with gait with head turns and decreasing dependency on assistive device.
Outcomes
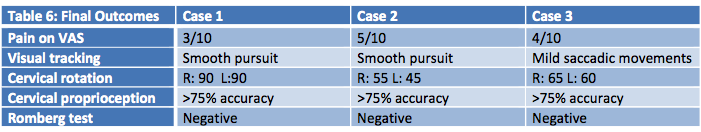
Most of the outcome measures used in this case series are of qualitative data, making it difficult for the researcher to determine the clinical significance of change in measures. It is noted that a clinically meaningful change in active cervical range of motion is between 5-10 degrees in patients with associated neck pain, which has significance in cases discussed. A minimal detectable change of three points, or 27% on the Numeric pain rating scale, is considered significant for neck pain. 3 Refer to Table 6 for final outcomes.
Case 1 was seen for a total of 20 visits. At the end of treatment, the patient reported 3/10 pain with shoulder or neck movements and was beginning to return to aerialist activities. The patient reported no bouts of dizziness or unsteadiness with her return to her prior level of function. She was very compliant with her home exercise program, and while she still has some strength deficits in her cervical and scapular region, it was not deemed medically necessary to continue with treatment and patient was subsequently discharged from therapy.
Case 2 was seen for a total of 15 visits. At the end of treatment, he had returned to playing football and was beginning to train for lacrosse, for his next activity. While returning to football, he had recurrent injuries to left sternocleidomastoid, which aggravated his condition and slowed his progression with therapy. His cervical range of motion and visual tracking ability improved; however, he still complained of 5/10 neck pain, especially after increasing activity level. The subject self-discharged due to financial difficulty.
Case 3 was seen in therapy for a total of 16 visits. At discharge, she was able to walk without an assistive device and had no incidents of falling since beginning therapy. She also reported decreased episodes of running into objects and decreased neck pain to 4/10. She still had increased muscular tone in the sternocleidomastoid and was able to perform more repetitive overhead activities without aggravating her condition. The patient was discharged due to reaching limits for insurance coverage.
Discussion
There is a great need for a diagnostic classification system to be adopted by the physical therapy profession to aid in the identification of cervicogenic dizziness. Currently, the research relies on subjective data and an exhaustive list of ruling out other pathologies. Subjective information including a combination of both cervical and vestibular pathology may be useful in steering the clinician towards identifying the diagnosis of cervical pathology. The location of pain may be a particular indicator for patients with combined vestibular pathology. The aims of the case series were to better identify the examination tests and measures that may be useful in identifying these patients, as well as describe the course of treatment.
Though there are many benefits to the case series study design, such as an ability to illustrate detailed examination, treatment progression, and work within the constraints of the clinic environment, it is important to note that one cannot assume a cause-and-effect relationship between physical therapy interventions and positive outcomes. So, while all three cases had positive outcomes using a hybrid treatment approach of manual and vestibular rehabilitation techniques, there may be other contributing factors to their success as well. Because a multi-factorial treatment approach was implemented, very few conclusions can be drawn to determine the effectiveness of one treatment over another. Further higher level case series and randomized control trials are needed to determine the benefits of a combination of vestibular and manual approach to treating these conditions.
Sources:
1.Armstrong, B, McNair P, et al. Head and Neck Position Sense. Sports Med. 2008: 38:101-117.
2.Fitz-Ritson D. Assessment of cervicogenic vertigo. ManipulativePhysiol Ther. 1991 ;14:193-198.
3. Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical pine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008; 38:640-645. http://dx.doi.org/10.2519/jospt.2008.2680
4. Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J orthop Sports Phys Ther, 2009; 39:364-377. http://dx.doi.org/10.2519/jospt.2009.2834
5. Lystad et al. Manual therapy with and without vestibular rehabilitation for cervicogenic dizziness: A systemic review. Chiropractice and manual therapies 2011; 19:21 1-11
6. Magnusson et al. Cervical muscle afferents play a dominant role over vestibular afferents during bilateral vibration of neck muscles. J Vest Res 2006;16: 127-136.
7. Norre ME. Cervical vertigo. Diagnostic and semiological problem with special emphasis upon “cervical nystagmus.”Acta Otorhinolaryngoly Belg. 1987;41:436-452.
8. Stratford, P. W. and Spadoni, G. (2001). The reliability, consistency, and clinical application of a numeric pain rating scale. Physiotherapy Canada 53(2): 88-91.
9. T. Bremner-Smith, A. J. Unwin, W. W. Williams. Sensory pathways in the spinal accessory
Nerve. J Bone Joint Surg [Br] 1999;81-B:226-8.
10. Toomingas A. Characteristics of pain drawings in the neck-shoulder region among the working population. Int Arch Occup Env Health. 1999;72:98–106.
11. Wapner. et. al.
12. Wriseley et al. Cervicogenic Dizziness: A review of diagnosis and treatment. J. Orth Sports Phys Ther 2000:30:755-766.